Service Details
Neuroophthalmology
Neuro-ophthalmology plays a vital role in diagnosing and treating visual problems linked to the brain and nervous system.
What is Neuro-Ophthalmology?
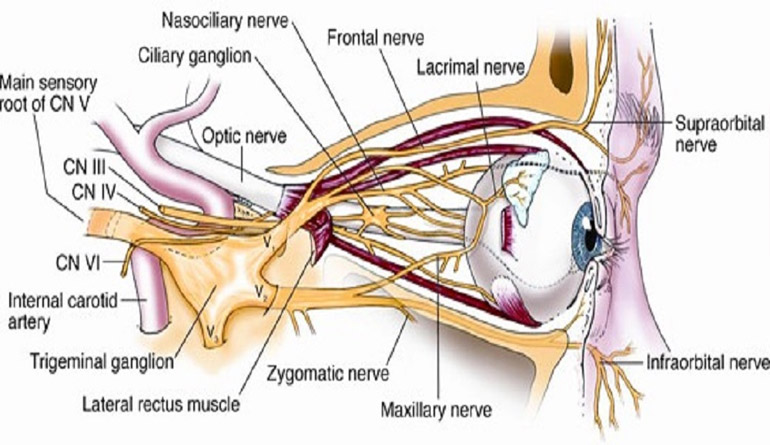
Neuro-ophthalmology is a specialized field of medicine that focuses on the relationship between the eyes and the brain, as well as the nervous system pathways that are critical for vision. This field combines neurology and ophthalmology to diagnose and treat visual problems that are related to the nervous system, including the optic nerve, brain, and muscles controlling eye movement. Neuro-ophthalmologists deal with complex conditions where vision problems are caused by neurological disorders rather than just issues within the eye itself.
(1).jpg)
The Role of Neuro-Ophthalmology
Neuro-ophthalmologists specialize in conditions that affect:
- Optic Nerve: Transmits visual information from the retina to the brain.
- Brain's Visual Processing Centers: Areas in the brain responsible for interpreting the signals received from the optic nerve.
- Eye Movement Control Centers: Regions in the brain and nervous system that coordinate the movement of the eyes.
Common Conditions Managed by Neuro-Ophthalmologists
-
Optic Neuritis:
Inflammation of the optic nerve, often associated with multiple sclerosis. Symptoms include sudden vision loss, pain with eye movement, and color vision changes. -
Papilledema:
Swelling of the optic nerve due to increased pressure inside the skull (intracranial pressure). This can be caused by brain tumors, hemorrhages, or severe head trauma and may lead to vision loss. -
Ischemic Optic Neuropathy:
Damage to the optic nerve due to poor blood supply, often associated with conditions like giant cell arteritis or cardiovascular disease. -
Ocular Myasthenia Gravis:
A neuromuscular disorder that causes weakness in the muscles controlling eye movements, leading to drooping eyelids (ptosis), double vision (diplopia), and difficulty with eye alignment. -
Stroke-Related Vision Loss:
Strokes can affect the visual processing areas of the brain, leading to vision loss, double vision, or visual field defects. -
Brain Tumors and Lesions:
Tumors or lesions in the brain can compress or damage the optic nerve or other visual pathways, causing a range of visual disturbances. -
Cranial Nerve Palsies:
Damage to the cranial nerves responsible for controlling eye movements can lead to eye misalignment, double vision, and difficulty moving the eyes. -
Hemianopia:
Loss of half of the visual field in one or both eyes, typically caused by brain damage from strokes, tumors, or trauma. -
Multiple Sclerosis (MS) and Other Demyelinating Diseases:
Conditions like MS can cause episodes of vision loss due to optic neuritis and can also lead to eye movement problems over time.
Symptoms Addressed in Neuro-Ophthalmology
Patients who need to see a neuro-ophthalmologist may experience a wide variety of symptoms, including:
- Sudden or progressive vision loss.
- Double vision (diplopia).
- Visual field loss (partial blindness in certain areas of the field of vision).
- Difficulty moving the eyes or coordinating eye movements.
- Abnormal pupil responses.
- Eye pain, especially with movement.
- Drooping eyelids (ptosis).
- Flickering vision or visual hallucinations (due to brain lesions).
- Headaches associated with visual disturbances.
Diagnostic Tools in Neuro-Ophthalmology
Neuro-ophthalmologists use a range of diagnostic tests to assess both the visual system and the brain's neurological functions, including:
-
Visual Acuity Testing:
Measures the sharpness of vision to detect any loss of clarity. -
Visual Field Testing (Perimetry):
Evaluates the full extent of the patient's visual field to identify areas of vision loss, such as hemianopia. -
Optical Coherence Tomography (OCT):
A non-invasive imaging test that provides detailed images of the optic nerve and retina, useful for diagnosing optic neuritis or optic neuropathy. -
Magnetic Resonance Imaging (MRI):
An MRI scan can help visualize the brain and optic nerve to detect lesions, tumors, or other neurological abnormalities affecting vision. -
Computed Tomography (CT) Scan:
Useful for assessing structural problems in the brain, including tumors, bleeding, or fractures. -
Electromyography (EMG) and Nerve Conduction Studies:
These tests assess the electrical activity of muscles and nerves, often used in conditions like myasthenia gravis. -
Lumbar Puncture (Spinal Tap):
May be used to measure intracranial pressure in cases of suspected papilledema or infections affecting the nervous system.
.jpg)
Treatment Options in Neuro-Ophthalmology
The treatment for neuro-ophthalmological conditions varies widely depending on the underlying cause. Some common treatments include:
-
Medications:
- Corticosteroids: Often used to reduce inflammation in conditions like optic neuritis or ischemic optic neuropathy.
- Immunosuppressants: In conditions like multiple sclerosis or autoimmune diseases, immunosuppressive drugs may be prescribed to control inflammation.
- Anticholinesterase Medications: For treating ocular myasthenia gravis, these medications help improve muscle function and reduce symptoms like double vision.
-
Surgery:
- Decompression Surgery: For conditions like papilledema, surgical intervention may be necessary to relieve pressure on the optic nerve or brain.
- Tumor Removal: If a brain tumor is affecting vision, neurosurgical removal or treatment is often necessary.
- Strabismus Surgery: For patients with cranial nerve palsies causing eye misalignment, surgery may be needed to restore normal eye movement.
-
Vision Therapy and Rehabilitation:
- Prism Glasses: To manage double vision caused by eye movement disorders.
- Vision Restoration Therapy (VRT): Helps train the brain to adapt to visual field deficits.
- Eye Patching or Occlusion Therapy: For patients with severe double vision, temporary occlusion of one eye can help manage symptoms.
-
Lifestyle Modifications and Monitoring:
- Regular monitoring and management of systemic conditions like hypertension, diabetes, or autoimmune diseases that can impact the optic nerve and visual system.
- Physical therapy or occupational therapy to assist with visual field loss or coordination problems.
Importance of Early Diagnosis and Treatment
Neuro-ophthalmological conditions often have complex causes and can lead to permanent vision loss if not addressed promptly. Early diagnosis and appropriate intervention are essential to preserving vision and preventing further neurological complications.